!.5 Million patients waited over 12 hours at A& - Patients waiting in ambulances
With more money going into the NHS to fund private healthcare companies taking over NHS care services, and the loss of NHS nurses and doctors to the privaate sector; the NHS is losing the battle to stop the levels of avoidable deaths taking place at A&Es, as patients wait in corridoers, on floors, and in Ambulances, and through errors in diagnosis.
Meanhwile, NHS Engalnd increases the number of non-doctors i.e. Physician Assistants who are being used instead of qualified doctors and nurses; and has already caused the deaths of at least two patients through mis-diagnosis and inappropriate treatment.
The Royal Collage Of Emergency Medicine's new report published today in two briefing documents, makes for very disturbing reading and is an endictment of Government policy of privatising the NHS in England and breaking it up into 42 Integrated Care Boards complete with budget and decision making autonomy.
One of the key elements in the briefing document entitled, Insights: Long Waits and Excess deaths, states:
'A large observational study of more than five million NHS patients showed an increase in all-cause 30-day mortality, adjusted for age and co-morbidity. This quantified the harm, demonstrating that there was one additional (excess) death for every 72 patients that spend 8-12 hours in the ED.'
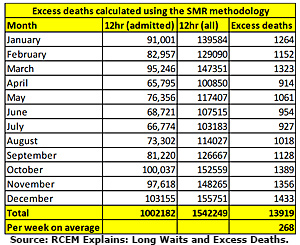 In the graph on the right, the RCEM estimated that over 13,000 pateints died in 2023 prematurely as a result of waits of over 12 hours to be diagnosed and treated!
In the graph on the right, the RCEM estimated that over 13,000 pateints died in 2023 prematurely as a result of waits of over 12 hours to be diagnosed and treated!
The report also states:
'It is important to note that this does not account for
patients that did not die but were nonetheless subject to increases in morbidity or inevitable worsening patient experiences due to delays.
Furthermore, patients delayed in the back of an
ambulance, of which there are thousands, are also
vulnerable to increased risk from delays, yet these
are not included in the figures. It is likely that these
are conservative estimations, and sadly the true scale of harm is difficult to quantify.'
Whilst the media is reporting on this, it does not identify the cause of the problem, nor does it question Government policy or ask the Government, 'where is the additional funding you claim is being put into the NHS; actually going?'
In a press release issued today and headed, Almost 300 deaths a week in 2023 associated with long A&E waits despite UEC Recovery Plan, the RCEM said:
New analysis by the Royal College of Emergency Medicine reveals that there were almost 300 deaths a week associated with long A&E waits in 2023.
That is despite the Government and NHSE implementing a Delivery Plan for the Recovery of Urgent and Emergency Care (UEC) services in January 2023 following the worse winter the health service has ever experienced.
The premise of the plan was to improve waiting times and patient experience by increasing capacity, growing the workforce, improving discharge, expanding care outside hospitals, and making it easier to access the right care.
Just over a year on RCEM has analysed progress against the plan and assessed what improvements have been made to recover emergency care services.
This work – shared with the Press Association and published today 1 April 2024 – reveals that in 2023, more than 1.5 million patients waited 12 hours or more, 65% of those were patients awaiting admission.
Using a method called the Standard Mortality Ratio – which calculates there will be one additional death for every 72 patients that experience an 8–12-hour wait prior to their admission – RCEM estimates that there were almost 14,000 associated excess deaths related to waits of 12 hours or longer in 2023 – more than 268 a week.
Scrutinising the other elements of the Delivery Plan the College also found that:
- Hospital Bed occupancy remains high, consistently averaging over 94%. More than an additional 11,000 available beds are required to achieve safe occupancy levels of 85%.
- The number of patients admitted into hospital has risen by 10% one year on.
- Recent figures show that a daily average of 13,690 patients remain in hospital after a decision to discharge them has been made, only 275 fewer than in January 2023.
- The percentage of answered calls to 111 that had clinical involvement has fallen from 43.6% in January 2023 to 40% in February 2024.
- In February 2024, only 56.5% of patients met the four-hour target, a fall of 1.5 percentage points compared to when the plan was announced.
 The college’s research has been published in two of its ‘RCEM Explains’ briefing documents – Progress Against Delivery Plan – one year and Insights: Long Waits and Excess deaths.
The college’s research has been published in two of its ‘RCEM Explains’ briefing documents – Progress Against Delivery Plan – one year and Insights: Long Waits and Excess deaths.
Dr Adrian Boyle, President of The Royal College of Emergency Medicine, said:
“We talk here about ratios and calculations, but it is vital to remember that each one of these deaths was of a person with loved ones and families who will forever be left asking ‘what if?’.
What if things had been different? If the system had functioned as it should? If waits in EDs were no longer than they should be?
And that is an awful position for them, and for the clinicians who have to deal with the realities of trying to provide the best possible care in such difficult and unacceptable circumstances.
The associated deaths figures rightly attracts the most attention but our analysis looked at the other elements of the UEC Delivery Plan also. It is vital that any initiatives are scrutinised, and their effectiveness assess so we can establish what is working and what needs adapting."
He concluded:
“Despite good intentions the plan has not been effective or has resulted in any consequential improvement.
What is needed is substantial investment and a commitment to resuscitating Emergency Care both for the clinicians battling with a struggling system and the patients who deserve so much better. We cannot continue with these inequalities in care, avoidable delays, and deaths.”
RCEM’s findings come with the following recommendations:
- Implementation of long-term plans to build additional capacity within the health and social care system.
- Ensure that hospitals never exceed 85% occupancy by opening additional staffed beds, so hospitals have the space and resources available to care for every patient.
- Performance-manage hospitals based on the proportion of patients waiting 12 hours or more from their time of arrival, alongside a four-hour target of 95%.
- Publish hospital-level performance figures to enable transparency and improve performance of hospital.
- Plans to implement RSV vaccination programmes should be accelerated for this coming winter.
- NHS Trusts should improve their staff vaccination programs for influenza and Covid-19.
RCEM continues to urge Government to embrace and act on the solutions cited in its manifesto to #ResuscitateEmergencyCare.
Read the full reports here: Insights: Long waits and excess deaths, Progress Against Delivery Plan – one year on
Source: RCEM
See also:
New Study Shows Healthcare Privatisation Harms Public Health
NHS Abolition/Privatisation News Archive


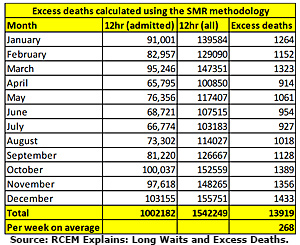 In the graph on the right, the RCEM estimated that over 13,000 pateints died in 2023 prematurely as a result of waits of over 12 hours to be diagnosed and treated!
In the graph on the right, the RCEM estimated that over 13,000 pateints died in 2023 prematurely as a result of waits of over 12 hours to be diagnosed and treated!